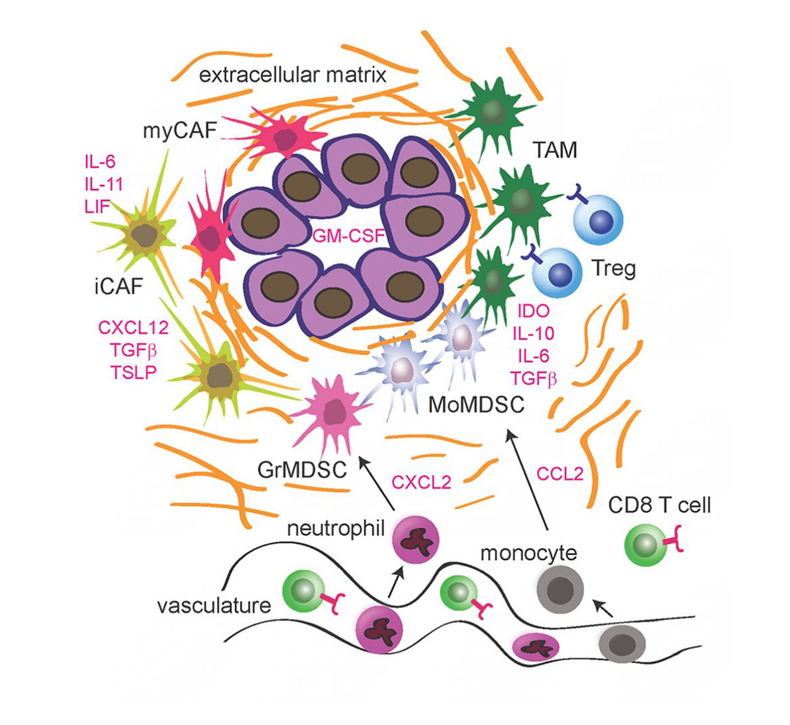
 The Pancreatic Cancer Tumor Microenvironment (TME). The immune-suppressive TME consists of myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAMs). Also shown are the extracellular matrix, vasculature, cancer-associated fibroblasts (CAFs), and major cytokines that have been implicated in TME regulation.
The Pancreatic Cancer Tumor Microenvironment (TME). The immune-suppressive TME consists of myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAMs). Also shown are the extracellular matrix, vasculature, cancer-associated fibroblasts (CAFs), and major cytokines that have been implicated in TME regulation.
While immunotherapy has shown promise in other solid tumors, e.g., lung cancer and melanoma, immune checkpoint inhibitors have thus far proven disappointing in pancreatic cancer.
Challenges Of Immunotherapy
The lack of efficacy of immunotherapy in pancreatic cancer patients is believed to be due to a relative dearth of neoantigens in pancreatic cancer cells as well as to an immune-suppressive tumor microenvironment (TME). The TME is composed of extracellular matrix (ECM), fibroblasts, and endothelial and hematopoietic cells, predominantly of the myeloid lineage. Most immune infiltrates from pancreatic cancer are largely devoid of cytotoxic effector T-cells due to the presence of myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAMs) which contribute to local immunosuppression within the tumor.
The Future Of Immunotherapy In PDAC
We envision a three-pronged approach of 1) chemotherapy/radiation to kill tumor cells releasing tumor neoantigens, 2) depletion/reprogramming of myeloid suppressor cells to relieve local immune-suppression, and 3) recruitment of T-cells/augmentation of T-cell responses. We hypothesize that a combination of immune-related agents will be found to be the first effective immunotherapy for pancreatic cancer.

